The CYPs are the cool genes on the block in pharmacogenomics testing, but in the background you’ll find a quiet but high achiever — the UGT1A1 gene.
Illustration by Sarah Nagorcka
Gene Dosage is a monthly column by Janan Arslan that finds out what genome science is uncovering about each individual's unique response to drugs and pharmaceuticals. Janan is a graduate student and pharmacogenomics researcher with a keen interest in personalised medicine.
Up to this point, CYPs have formed the foundation of my columns, and there is no doubt this trend will continue in the future. However, this month I wanted to talk about an unsung hero ‒ a gene that is not readily available in all pharmacogenomics testing companies (but perhaps it should be). I speak of the UGT1A1 gene. The test for UGT1A1 is useful both pharmacologically and biologically ‒ it not only indicates the metabolism activity of drugs, such as cancer drug irinotecan, but it also provides insight into various diseases.
UGT1A1 is a clean, abbreviated version of its full name: UDP glucuronosyltransferase (UGT) 1 family, polypeptide A1 (1A1). Try saying that ten times really fast. Genes that belong to the UGT family code for an enzyme that performs glucuronidation, a chemical reaction in which glucuronic acid, a derivative of glucose, is conjugated (attached) to substances. One substance that undergoes this process is bilirubin, which is formed when your red blood cells are broken down. In its unconjugated (unattached) form, bilirubin is toxic. The addition of glucuronic acid creates a non-toxic form of bilirubin, allowing it to be dissolved in bile and easily excreted.
Although less commonly tested than the CYPs, the UGT1A1 gene stands out. rawdonfox/Flickr (CC BY 2.0)
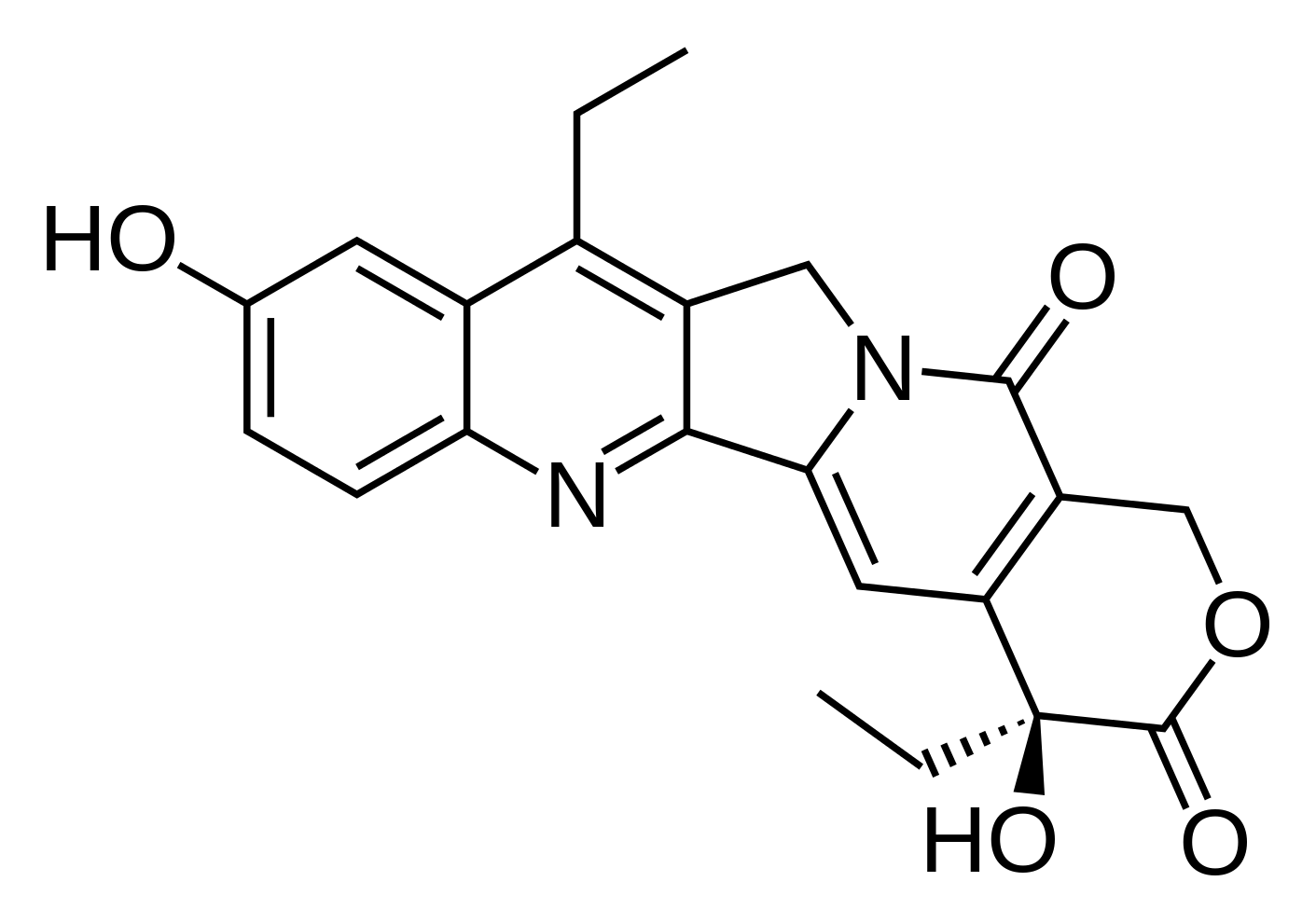
In addition to bilirubin, SN-38 is another substance subject to glucuronidation. SN-38 is the active metabolite of irinotecan, an anti-cancer agent used for the treatment and prevention of tumour cells. Irinotecan is first converted to SN-38 by the liver, before being glucuronidated into its inactive form by UGT1A1.
Patients with a genetic variant for UGT1A1 will have decreased glucuronidation and increased levels of SN-38, which has strong anti-tumour effects. So why is it important that our bodies be able to convert this metabolite to its inactive form? In reality, elevated levels of SN-38 can make the patient susceptible to bone marrow and gastrointestinal toxicities. Patients may experience symptoms like diarrhoea or, worse, myelosuppression, where a reduction of bone marrow reduces white and red blood cells and platelets, and therefore lowers immunity.
The US Food and Drug Administration have established UGT1A1’s use in personalised medicine. Besides irinotecan, other drugs such as arformoterol and indacaterol (bronchodilators/inhalers), and nilotinib and pazopanib (anti-cancer drugs) have drug labelling information that includes UGT1A1-related warnings.
While irinotecan, arformoterol, and indacaterol use UGT1A1 in their metabolic processes, pazopanib and nilotinib act as inhibitors of the UGT1A1 gene. An inhibitor is a drug that can alter the function of a gene. So in this instance, if a patient were to use pazopanib or nilotinib, that would affect the function of their UGT1A1 gene, limiting their ability to metabolise drugs like irinotecan.
The SN-38 metabolite can either make or break you. Fvasconcellos/Wikimedia Commons (public domain)
Decreased UGT1A1 activity has also been associated with constitutional jaundice known as Crigler-Najjar syndrome and Gilbert's syndrome. Crigler-Najjar syndrome is considered the most severe manifestation of UGT1A1 genetic variation, as it results in elevated levels of unconjugated bilirubin. As is characteristic with jaundice, patients with Crigler-Najjar have yellowish eyes and skin. There are two types of Crigler-Najjar syndrome. Individuals with type I have no enzyme function, while those with type II have reduced enzyme function (approximately 20%). As a result, type I patients have greater signs and symptoms than type II patients, since they have no ability to convert bilirubin to its conjugated form. The toxic substance therefore builds up in their system.
Patients with Gilbert’s syndrome are characterised as having periods of mild and chronic unconjugated bilirubin. Sufferers of Gilbert’s syndrome have only 30% enzyme function.
The most common mutation that causes all this is the addition of an extra piece of DNA (known as “TA”) to the promoter region of the UGT1A1 gene (known as the “TATA” sequence). This addition affects the synthesis of DNA, as the promoter region is near the beginning of the DNA and considered to be a binding site where DNA synthesis begins.
When an enzyme has an altered binding site, its usual function can’t be unlocked. Mario Klingemann/Flickr (CC BY-NC 2.0)
My best analogy to describe how mutations affect enzyme function goes something like this. Think of the enzyme as a lock, and the substance that is processed by that enzyme as a key. For the enzyme to function at full capacity, the key needs to fit into the lock. If there are no mutations, the lock is in perfect condition, and the key and lock both fit well. However, if there is a mutation that physically alters the lock in a way that the key no longer fits, then the lock is rendered useless.
Similarly, there is a site on an enzyme that the substance must lock onto for it to work. A mutation alters that site, making it more difficult for the substance to latch on. This leads to reduced enzymatic activity, as the enzyme and substance cannot completely connect. Genetically, we most commonly identify this abnormality in the form of a genotype called UGT1A1*28.
Much like its more popular and commonly known cousins, the CYPs, UGT1A1 plays a pivotal role in explaining drug metabolism. While I did not see this test offered at every place of employment (generally related to available technologies), the UGT1A1 test is one I hope you will soon be able to find at your nearest friendly neighbourhood pharmacogenomics testing company.
Edited by Andrew Katsis and Ellie Michaelides